Healthcare disparities in minority communities rise during pandemic
Studies and statistics have shown that the healthcare system in the U.S. has shown start disparities between white and minority communities.
May 7, 2021
Amid the COVID-19 pandemic, trust in the American healthcare system has been higher than ever. The United States has one of the highest death rates due to COVID-19 across the world, and its mortality rates will likely increase. Due to the international spread of COVID-19, we may see diverging rates of mortality, disease outcome, and access to healthcare between the U.S and other countries. This has opened American’s eyes to many disparities in healthcare due to race.
According to KFF, health and health care disparities refer to differences in health and health care between groups that are closely linked with social, economic, and/or environmental disadvantage. Disparities in healthcare occur across socioeconomic status, age, geography, language, gender, disability status, citizenship status, and sexual identity and orientation.
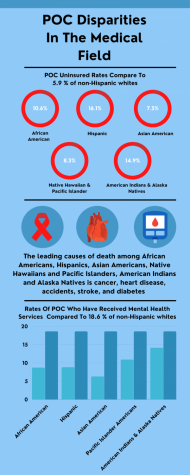
Insured vs Uninsured
According to the Brookings Institution, prior to implementation of the Affordable Care Act (ACA), nearly one in three Hispanic Americans and one in five Black Americans were uninsured. Since the ACA’s core coverage provision came into effect in 2014, uninsured rates fell across all racial and ethnic groups, with the biggest gains among Black and Hispanic people.
Still, 30 million people remain uninsured. About half of those 30 million are people of color. Fourteen states have refused to expand Medicaid under the ACA, which is one of the reasons why people of color are disproportionately likely to be uninsured today. More than 90 % of people who don’t have insurance because their state did not expand Medicaid live in the south.
According to CAP
- In 2017, 10.6 %of African Americans were uninsured compared with 5.9 % of non-Hispanic whites.
- In 2017, 16.1% of Hispanics were uninsured compared with 5.9 % of non-Hispanic whites.
- In 2017, 7.3 % of Asian Americans were uninsured compared with 5.9 % of non-Hispanic whites.
- In 2017, 8.3% of Native Hawaiians and Pacific Islanders were uninsured compared with 5.9% of non-Hispanic whites.
- In 2017, 14.9 %of American Indians and Alaska Natives were uninsured compared with 5.9% of non-Hispanic whites.
Health Conditions
Throughout the advances in diagnosis and treatment of most chronic diseases, there is evidence that racial and ethnic minorities tend to receive a lower quality of care and have poorer health.
African Americans or Black Americans
According to CAP
- 13.8% of African Americans reported having fair or poor health compared with 8.3 % of non-Hispanic whites.
- Eighty percent of African American women are overweight or obese compared to 64.8 % of non-Hispanic white women.
- The leading causes of death among African Americans are heart disease, cancer, and accidents.
- There are 11 infant deaths per 1,000 live births among Black Americans. This is almost twice the national average of 5.8 infant deaths per 1,000 live births.
Hispanic Americans or Latinx Americans
According to CAP
- Ten percent of Hispanics reported having fair or poor health compared with 8.3 % of non-Hispanic whites.
- Approximately Twenty-five percent of Hispanics have high blood pressure.
- The leading causes of death among Hispanics are cancer, heart disease, and accidents.
- There are 5.1 infant deaths per 1,000 live births among Hispanic and Latinx Americans.
Asian Americans
According to CAP
- In 2017, tuberculosis was 35 times more common in Asian Americans than among non-Hispanic whites.
- Asian Americans are twice as likely to develop chronic hepatitis B than non-Hispanic whites and are eight times more likely to die from hepatitis B than non-Hispanic whites.
- The leading causes of death for Asian Americans include cancer, stroke, heart disease, accidents, and diabetes.
- There are 3.8 infant deaths per 1,000 live births in this population.
 Native Hawaiian or other Pacific Islander Americans
Native Hawaiian or other Pacific Islander Americans
According to CAP
- Native Hawaiians and Pacific Islanders have higher rates of smoking, alcohol consumption, and obesity in comparison to other populations.
- The incidence rate of tuberculosis for Native Hawaiians and Pacific Islanders is higher than in any other population.
- The leading causes of death for Native Hawaiians and Pacific Islanders include cancer, heart disease, accidents, stroke, and diabetes.
- There are 7.6 infant deaths per 1,000 living births in this population.
American Indians and Alaska Natives
According to CAP
- 17.4 %of American Indians and Alaska Natives reported having fair or poor health compared with 8.3 % of non-Hispanic whites.
- American Indian and Alaska Native youth and adults have the highest rates of cigarette smoking among all racial and ethnic groups in the United States.
- The leading causes of death among American Indians and Alaska Natives are heart disease, cancer, and accidents.
- There are 9.2 infant deaths for every 1,000 living births in this population.
Mental Health
Racial disparities, or unfair differences, within the system of mental health are well documented. Research indicates that compared with people who are white, black, indigenous and people of color are:
- Less likely to have access to mental health services
- Less likely to seek out services
- Less likely to receive needed care
- More likely to receive poor quality of care
- More likely to end services prematurely
African Americans or Black Americans
According to CAP
- In 2018, 8.7 %of African American adults received mental health services compared with 18.6 % of non-Hispanic white adults.
- 6.2 percent of African American adults received prescription medication for mental health services compared with 15.3% of non-Hispanic white adults.
Hispanic Americans or Latinx Americans
According to CAP
- In 2018, 8.8% of Hispanic adults received mental health services compared with 18.6 % of non-Hispanic white adults.
- 6.8% of Hispanic adults received prescription medication for mental health services compared with 15.4 %of non-Hispanic white adults.
Asian Americans
According to CAP
- In 2018, 6.3 % of Asian American adults received mental health services compared with 18.6 % of non-Hispanic white adults.
- 3.6 percent of Asian American adults received prescription medications for mental health services compared with 15.4 % of non-Hispanic white adults.
Native Hawaiian or other Pacific Islander Americans
According to CAP
- 10.9 % of Native Hawaiian and Pacific Islander adults received mental health services in 2018 compared with 18.6 % of non-Hispanic white adults.
- 6.3 % of Native Hawaiian and Pacific Islander adults received prescription medication for mental health services in 2018 compared with 15.4 % of non-Hispanic white adults.
American Indians and Alaska Natives
According to CAP
- 14.1 % of American Indian and Alaska Native adults received mental health services compared with 18.6 percent of non-Hispanic white adults.
- 11.6 % of American Indian and Alaska Native adults received prescription medication for mental health services compared with 15.4 percent of non-Hispanic white adults.
These statistics shed light on the American healthcare system as a whole. According to The Commonwealth Fund, the U.S. spends more on health care than any other country, yet has the lowest life expectancy and highest suicide rates among the 11 nations. Compared to peer nations, the U.S. has among the highest number of hospitalizations from preventable causes and the highest rate of avoidable deaths. The U.S, since its beginning has been under fire for its treatment of its POC citizens, that bias is starting to show through its healthcare. We must recognize that the poor state of the American healthcare system is not just a money issue, it’s also a race issue.